Have you ever been surprised to find your stool or toilet bowl water tinged with red after passing a bowel movement? Or perhaps your toilet paper is streaked with blood after wiping?
While blood in any situation can be concerning, it can be especially so when it’s occurring with a bowel movement. You may immediately assume that the blood is from hemorrhoids, swollen veins that sit around the anus and lower rectum. However, while hemorrhoids can cause bleeding, they don’t always. And they’re also not the only condition that can cause blood in your stool.
In this blog, we’ve outlined the differences and similarities between hemorrhoids and blood in stool so that you can feel more secure in what to expect and what to do next.
Hemorrhoids
Hemorrhoids are swollen veins that can be external, developing under the skin around the anus, or internal, developing inside the rectum. These two types can cause some differences in symptoms.
Internal hemorrhoids are typically not visible or palpable and rarely provoke discomfort. However, you may have painless bleeding during a bowel movement, which appears as bright red blood on toilet paper or in the toilet. In some cases, an internal hemorrhoid may push through the anal opening, which can cause pain and irritation.
External hemorrhoids are often the type that are more noticeable, and they can cause symptoms such as:
- Pain or discomfort
- Itching
- Irritation in the anal region
- Bleeding
- Swelling around the anus.
Hemorrhoids aren’t the only cause of bleeding
While bleeding is a possible symptom of hemorrhoids, it does not always occur, and perhaps more importantly, hemorrhoids are not the only gastrointestinal condition that can cause blood in stool. This is why it is important to determine the cause of blood in your stool.
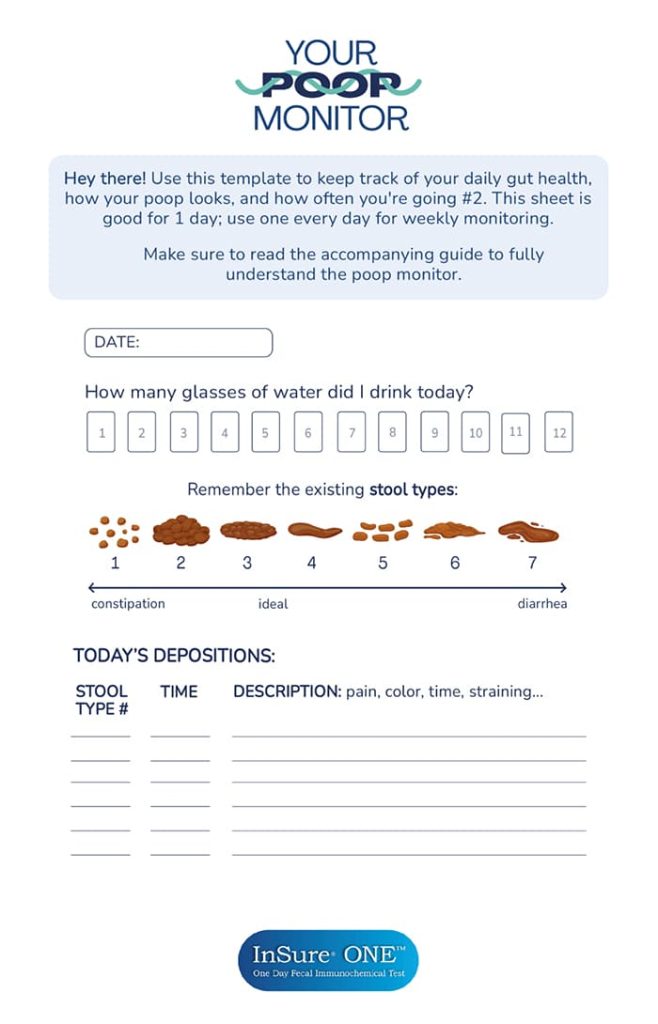
Additionally, while some of these conditions that cause blood in stool have other symptoms, like constipation, diarrhea, or abdominal pain, they don’t always. Even more, the blood may not always be visible, making it even harder to detect them. This is why screening tools, such as a fecal immunochemical test (FIT), are vital for detecting even microscopic amounts of blood.
With life-altering diseases such as colorectal cancer causing hidden blood in the stool, detecting this blood can result in months-earlier treatment, which can significantly increase the likelihood of successful treatment.
Causes and Shared Risk Factors
Hemorrhoids are generally formed because of increased pressure in the lower rectum from straining during bowel movements, chronic diarrhea, obesity, pregnancy, eating a low-fiber diet, etc.
As for Blood in Stool, it may be caused by several conditions, such as hemorrhoids, rectal ulcers, anal fissures, diverticulitis, inflammatory bowel diseases, or colorectal cancer.
Notably, inflammatory bowel diseases can often cause bouts of constipation or diarrhea, which can then increase the risk of hemorrhoids. In this case, both blood in stool and hemorrhoids would have the same root cause, the inflammatory bowel disease.
Additionally, the risk of hemorrhoids increases with age, since the tissues around the veins at the end of the gastrointestinal tract can weaken and stretch. Age also increases the risk of colorectal cancer, another cause of blood in stool.
Diagnosis
If the hemorrhoids are external, a healthcare provider may be able to see them. As for internal hemorrhoids, they may be diagnosed using a digital or visual inspection of the anal canal and rectum to look or feel for anything unusual.
Blood in stool can be detected using a fecal immunochemical test (FIT) or guaiac fecal occult blood test (gFOBT). However, these tests cannot diagnose the cause of the blood. A colonoscopy is often used for this, as it allows a doctor to inspect your entire colon.
Even with hemorrhoids, if your doctor feels that your symptoms suggest another digestive system disease or if you have risk factors for colorectal cancer, they may recommend a colonoscopy.
Treatments and Management
Hemorrhoids can often be treated using at-home remedies and lifestyle changes, such as:
- Eating high-fiber foods to avoid straining on the toilet
- Using topical treatments to manage the pain
- Taking pain relievers by mouth (prescribed by a healthcare provider)
- Soaking in a warm bath or sitz bath for 10-15 minutes two to three times a day.
In cases of severe hemorrhoids, such as those with a blood clot, surgical interventions may be necessary.
If blood is detected in stool through screening tests, a healthcare provider will generally recommend completing a colonoscopy to determine the cause of the blood, which will then dictate the treatment or management methods recommended.
Complications and Risks
While complications from hemorrhoids are rare, they may include anemia from ongoing blood loss, strangulated hemorrhoids (which can cause extreme pain), or a blood clot (forming a thrombosed hemorrhoid).
In comparison, the complications that may arise from having blood in your stool depend on the condition causing the bleeding and the repercussions of a lack of diagnosis and treatment.
For instance, if colorectal polyps are causing the blood in stool, there is a risk of them becoming cancerous if they continue to grow. If the blood is from an inflammatory bowel disease, some complications include severe dehydration, blood clots, and colon cancer.
Ultimately, whether the blood is from hemorrhoids or another condition, it’s best to see a doctor to determine the cause of the blood if it’s unknown and begin treatment, if necessary.
When To Seek Medical Attention
If you ever notice any of the following signs, it’s recommended to seek medical attention:
- Bleeding before, during, or after bowel movements
- Hemorrhoid discomfort that does not resolve in a week
- Worsening pain
If you have severe abdominal pain or cramping or the bleeding is continuous or heavy, seek immediate medical attention.
In general, whenever you have blood in your stool, it’s best to reach out to a healthcare provider to determine the cause. While most cases of hemorrhoids can be easily managed independently, other causes of blood in stool may require medical interventions. Diagnosing them sooner rather than later is preferable.
To take back control of your health and monitor for hidden blood in your stool, try the InSure ONE Test. Gain a better understanding of your gastrointestinal system and have the tools needed to get prompt medical care.
References
- Definition & Facts of Hemorrhoids. (2024). National Institute of Diabetes and Digestive and Kidney Diseases; NIDDK – National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids/definition-facts
- Hemorrhoids. (2023). Medlineplus.gov; National Library of Medicine. https://medlineplus.gov/hemorrhoids.html
- Sabry AO, Sood T. Rectal Bleeding. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563143/