Menopause, marked by a significant drop in estrogen levels, ends monthly periods and brings common symptoms like hot flashes, bladder control issues, mood changes, and painful intercourse. However, digestive issues such as bloating, constipation, and incomplete digestion are often overlooked but can cause daily discomfort, impacting your quality of life.
The Gut-Hormone Connection
The connection between your gut health and hormonal balance is bidirectional, meaning poor gut health throws your hormonal balance out of whack, and having unbalanced hormones can negatively affect your gut.
This is because the digestive process relies on hormones to do its job, and hormones need to be in balance in order to function properly. If even one area is too high or too low, the repercussions can snowball.
While there are some hormones strongly associated with the digestive system, such as gastrin or leptin, other hormones that you may not expect, such as female sex hormones and stress hormones, also influence the GI system. Depending on the hormone, their presence may help or hinder your gut health.
For instance, estrogen has been shown to be involved in gut motility and pain sensitivity. It also plays a role in the production of stomach acid, which aids in the breakdown of food. With these roles, estrogen helps to move the digestive system along.
Progesterone, however, has the opposite effect, as it is shown to slow digestion.
Stress hormones such as cortisol can also affect your gut health, with high cortisol levels shown to cause inflammation in the digestive tract and throw off the microbiome’s balance. Additionally, stress can influence the muscles in your intestines, which can keep your bowels from removing harmful gut bacteria.
Knowing that menopause causes a significant change in hormone levels and that these hormones can influence our gut, it should come as no surprise that menopause can also affect the health of your gut.
Symptoms and Impact
The declining hormone levels during menopause can also cause digestive issues, such as:
- Bloating
- Gas
- Constipation
- Incomplete digestion
It’s not just a decline in hormones that we see during menopause, either: the stress hormone, cortisol, steadily rises during the late stage of menopause. Cortisol can cause inflammation in the digestive tract, which can make GI conditions such as IBS, Crohn’s disease, ulcerative colitis, and GERD worse
Cortisol can also cause an imbalance in your gut microbiome, which can exacerbate GI conditions and suppress your immune system, making you more likely to get sick.
Overall, even hormones that are not typically associated with the gut can influence the body’s second brain.
Management and Solutions
Changing hormone levels may be an unavoidable part of menopause, but there are tips you can follow to manage the digestive issues that pop up.
Diet
Since your diet is what directly travels through the gastrointestinal system, you hold a lot of power over your symptoms simply through what you eat and drink.
– Stay Hidrated
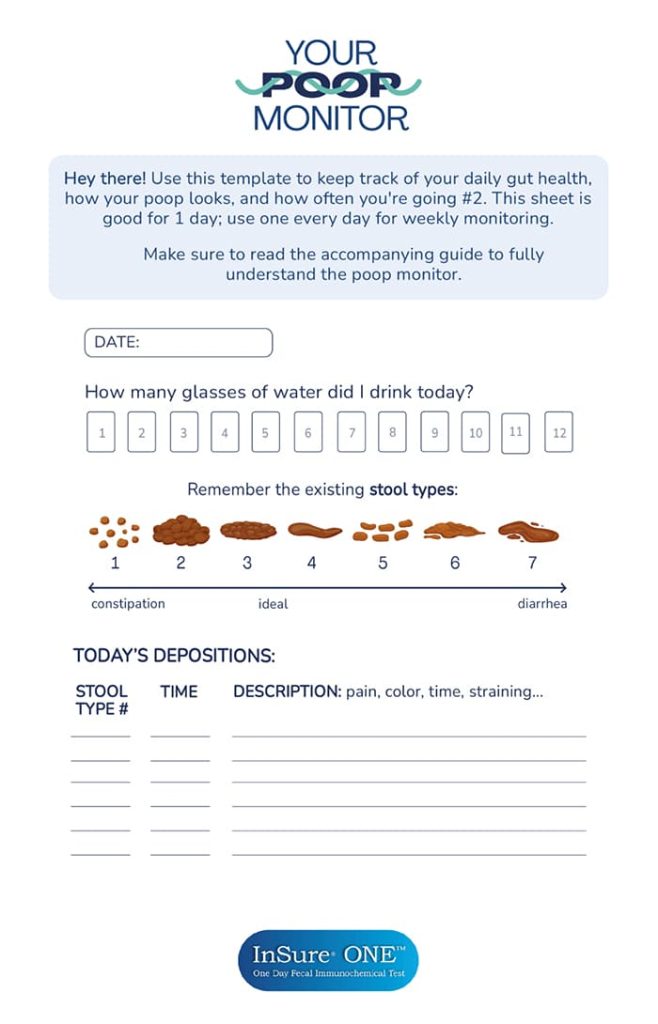
The number one tip to improve your GI health is to stay hydrated. Your body uses water to break down and process food, which allows you to absorb all its nutrients. Additionally, water can help soften your stool. With constipation a common side effect of menopause because of low estrogen levels, water’s ability to soften stool is a huge help.
– Fiber Up
Yet another way that you can prevent constipation is by eating enough fiber. There are two types—soluble and insoluble—and they both serve an important purpose. Soluble fiber dissolves in water to make a gel-like consistency that lowers blood cholesterol and glucose levels. Insoluble fiber helps to move your digestive system along, which is helpful for those with constipation.
The Institute of Medicine recommends that women 50 or younger aim for 25 grams of fiber per day, and those who are 50 or older aim for 21 grams. Some of the best sources of fiber include fruits, vegetables, whole grains, beans, and nuts.
– Avoid Processed Foods
To further reduce the likelihood of constipation, avoid processed foods; they’re typically higher in fats, which are harder to digest.
– Natural Remedies
Probiotics and digestive enzymes are two supplements that can further support your digestive system, especially when dealing with menopause and digestive problems. Probiotics help to replenish the diverse microbiome found in your gut—which cortisol can deplete—and digestive enzymes help your body break down food more easily.
Before starting any supplements, though, it’s best to check with a doctor to see if there is a need for supplementation or if your deficiency or gastrointestinal symptoms are due to a medical cause that should be diagnosed. Even if you plan to take over-the-counter supplements, you should still check with your doctor first. Most people don’t need supplements, so your doctor can help you determine if they will benefit you.
Screen For Gut Health
Menopause bloating, along with constipation, menopause headaches, and incomplete digestion, are common symptoms that can arise during menopause. These gastrointestinal issues may also indicate other underlying health conditions. To effectively identify and address any concerns, a simple at-home stool test like the InSure ONE. can be a valuable tool. This test detects hidden blood in the stool, even if it’s not visible to the naked eye
Blood in your stool may be a sign of hemorrhoids, IBS, colorectal polyps, or even colorectal cancer, so detecting blood earlier allows for prompt treatment.
Stay Proactive During Menopause
The risk of these conditions can increase when you have menopause, with the risk of colon cancer increasing by 1.5 times in menopausal women. In addition to a regular FIT, be sure to keep an eye out for any symptoms of colorectal cancer, such as diarrhea, constipation, blood in or on the stool, abdominal pain or cramps, and unexplained weight loss.
Menopause may increase your risk of GI concerns, but you can stay proactive in your colorectal health by focusing on your diet, supplementing (when needed), and regularly screening for GI concerns such as colorectal cancer.
References
- Woods, N. F., Mitchell, E. S., & Smith-Dijulio, K. (2009). Cortisol levels during the menopausal transition and early postmenopause: observations from the Seattle Midlife Women’s Health Study. Menopause (New York, N.Y.), 16(4), 708–718. https://doi.org/10.1097/gme.0b013e318198d6b2
- Trumbo, P., Schlicker, S., Yates, A. A., & Poos, M. (2002). Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. (Commentary). Journal of the American Dietetic Association, 102(11), 1621–1631. https://go.gale.com/ps/i.do?id=GALE%7CA94870700&sid=googleScholar&v=2.1&it=r&linkaccess=abs&issn=00028223&p=AONE&sw=w&userGroupName=anon%7Ea24d5cf3&aty=open-web-entry
- Vecchia, C. L. (1991). Book review. Annals of Oncology, 2(2), 92. https://doi.org/10.1093/oxfordjournals.annonc.a057890
- Alqudah, M., Al-Shboul, O., Al Dwairi, A., Al-U´Datt, D. G., & Alqudah, A. (2022). Progesterone inhibitory role on gastrointestinal motility. Physiological research, 71(2), 193–198. https://doi.org/10.33549/physiolres.934824
- Cherpak C. E. (2019). Mindful Eating: A Review Of How The Stress-Digestion-Mindfulness Triad May Modulate And Improve Gastrointestinal And Digestive Function. Integrative medicine (Encinitas, Calif.), 18(4), 48–53.